Off the Record: Groundbreaking Study Links Gut Health to Autism Risk — Starting in the Womb

In recent years, the gut microbiome has emerged as a key player in human health, influencing everything from our emotional responses and metabolism to immune function and even brain development. Now, a new study published in The Journal of Immunology adds another layer to this complex picture—suggesting that a mother’s gut health may play a significant role in the risk of developing autism spectrum disorder (ASD).
A Closer Look at the Gut-Brain Connection
While previous studies have linked gut bacteria to mood disorders and autoimmune diseases like lupus and type 1 diabetes, this latest research explores its connection to autism, a neurodevelopmental condition that affects communication, behavior, and social interaction.
According to John Lukens, PhD, lead researcher from the University of Virginia School of Medicine, “The microbiome is really important to the calibration of how the offspring’s immune system is going to respond to an infection, injury, or stress. It can shape the developing brain in multiple ways.”
But here's the striking twist: the study suggests it’s not the child’s own microbiome that has the most impact—it’s the mother’s.
The Molecule That May Hold the Key: IL-17a
Central to this groundbreaking study is interleukin-17a (IL-17a), a molecule produced by the immune system. IL-17a has already been associated with autoimmune diseases like psoriasis, rheumatoid arthritis, and multiple sclerosis, and plays a vital role in fighting infections—particularly fungal ones. But recent findings show it also influences brain development in the womb.
To test its role in autism-like conditions, researchers used mice from two different lab environments. One group had gut microbiota that heightened the inflammatory effects of IL-17a, while the second group acted as the control, lacking this inflammation-inducing gut flora.
What They Found Was Stunning
When IL-17a was suppressed in both groups, all mouse pups were born with normal, neurotypical behavior. However, when left untreated, the offspring of the first group—whose mothers had inflammation-prone microbiomes—began to develop behaviors resembling autism, including impaired social interaction and repetitive actions.
To confirm the microbiota’s influence, researchers performed a fecal transplant from the first group’s mothers to the second. The result? The second group’s offspring, now carrying similar gut flora, also developed autism-like symptoms.
Implications for Autism Research
Although these findings are based on animal models and cannot yet be directly applied to humans, the implications are profound. They suggest that a mother’s gut health during pregnancy may significantly influence the neurological development of her child.
“This is only the beginning,” Lukens notes. “We now need to determine which specific aspects of the maternal microbiome contribute to autism risk and whether these patterns can be detected in human pregnancies.”
IL-17a may be just one piece of a much larger puzzle—there are likely multiple immune pathways and microbiota interactions involved.
What’s Next?
As researchers continue to map the microbiome’s influence on the brain, this study opens the door to new preventive strategies for neurodevelopmental disorders. If similar patterns are found in humans, it could eventually lead to gut-targeted therapies for pregnant women—aimed at supporting healthier neurodevelopmental outcomes in their children.
For now, this research highlights a growing scientific consensus: the path to brain health may begin in the gut—and possibly even before birth.
News in the same category
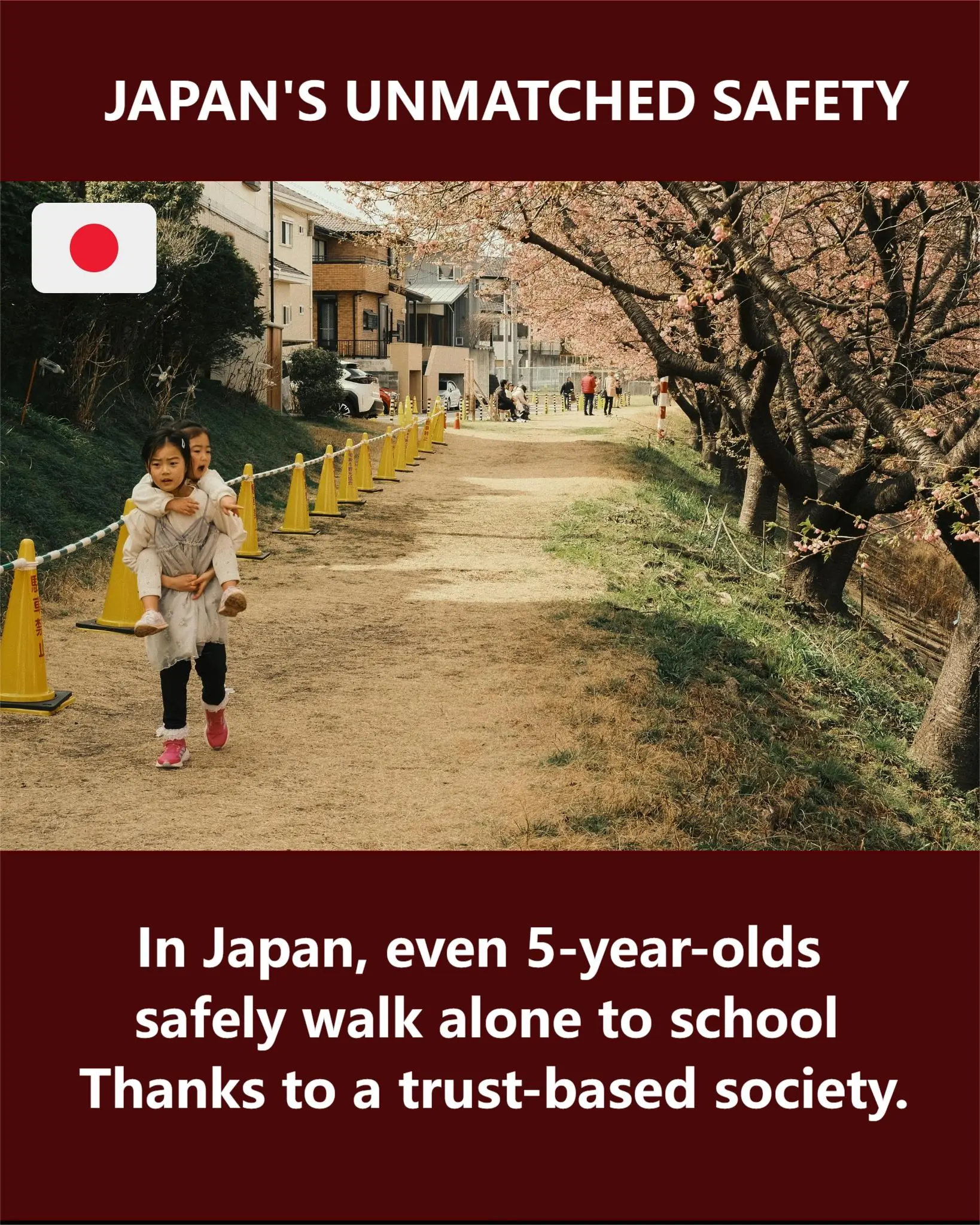
Japan: Where Even 5-Year-Olds Can Walk to School Alone

Deformed dog that can’t eat set to be euthanized: When the truth is uncovered, vet makes the correct decision

Boxer puppy collapses in stranger’s driveway looking for help

Homeless lady given free ‘ugly’ abandoned trailer, but wait till you see what she made of it

Your Pillowcase Could Be Dirtier Than a Toilet Seat: Here's Why It Matters
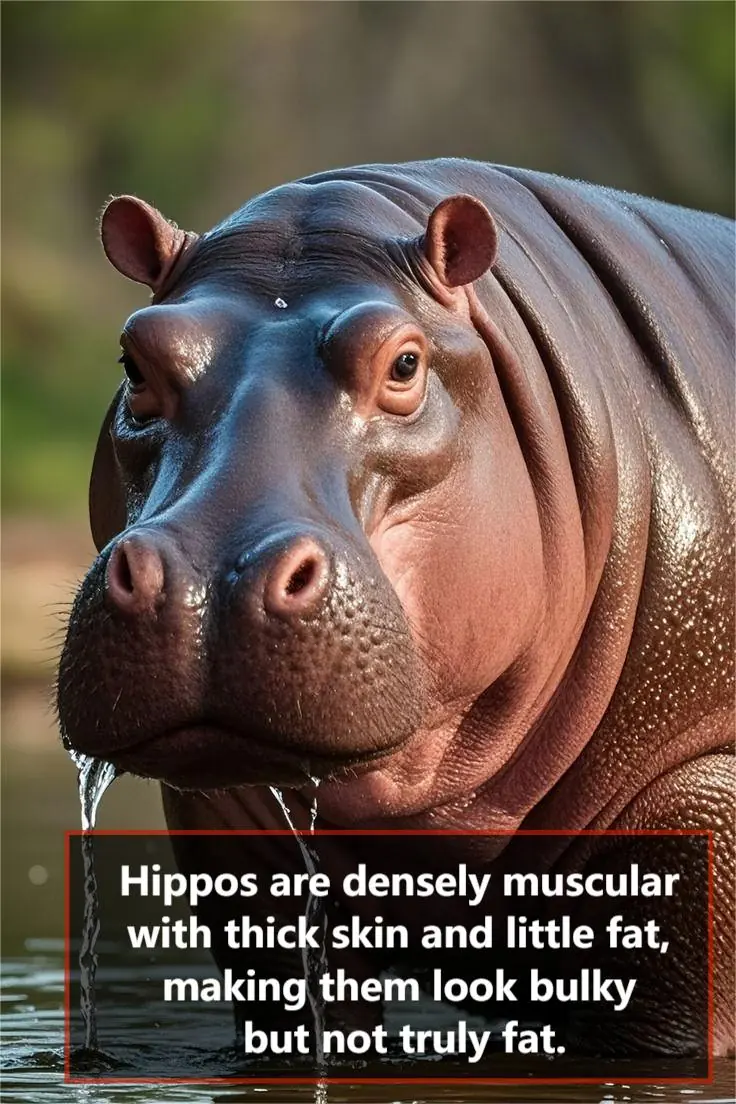
Hippos: Surprisingly Muscular Giants, Not Fat Creatures

Why Do Couples Sleep Separately After 50? The Real Reason Might Surprise You

Astronomers Discover Mysterious Space Beacon Sending Pulses Every 44 Minutes
The terrifying reason cruise ship passengers are asked to turn off lights and close curtains when traversing specific waters

This ex-child star left Hollywood for motherhood and is now a 60-year-old mom of six and proud grandmother

Parents plan funeral for 10-yr-old with cancer – She then opens her eyes and says something that leaves them stunned
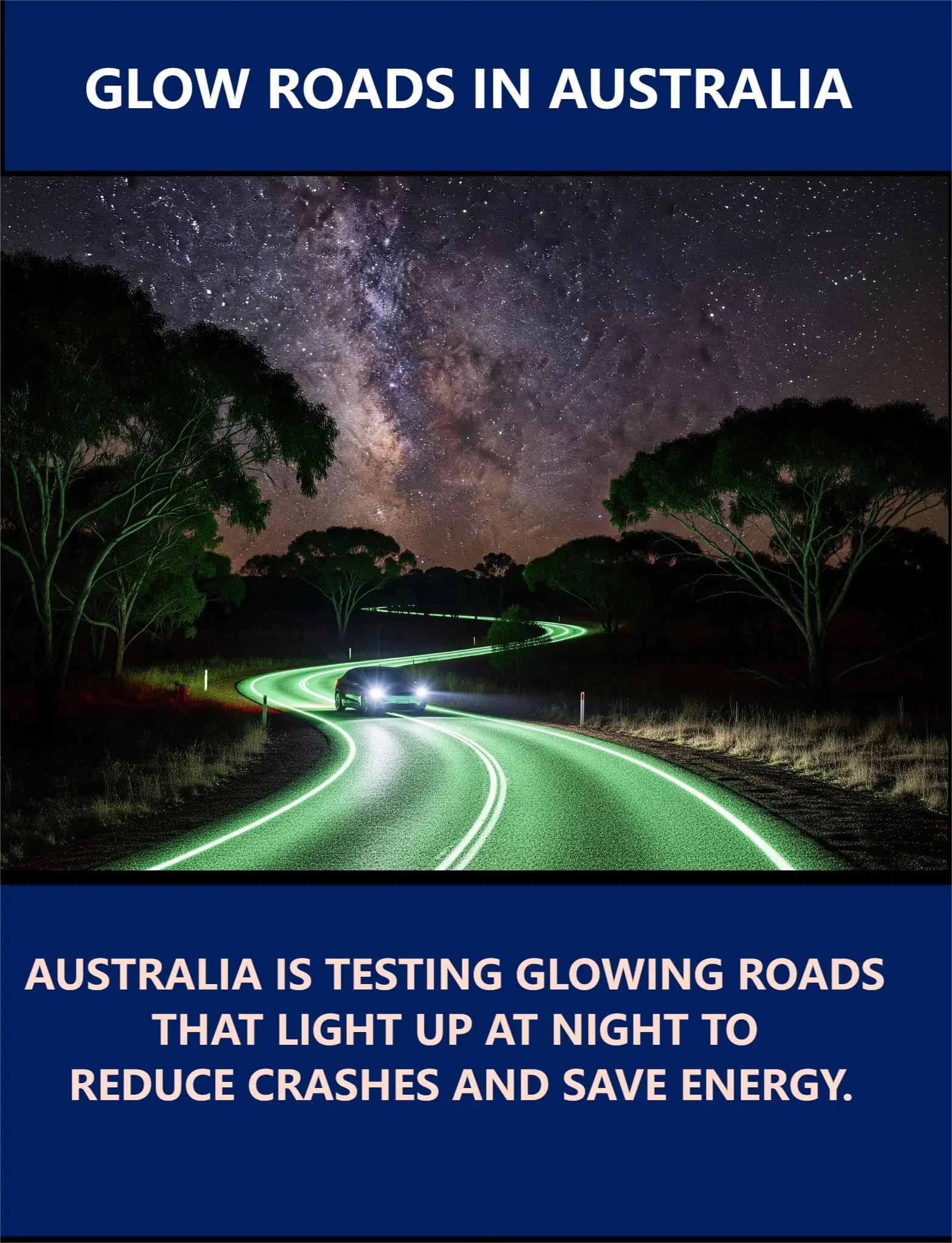
Australia Trials Glow-in-the-Dark Roads to Boost Nighttime Driving Safety

Ex-model on addiction and homeless life: ‘I’m in a lot of pain’

Twin toddlers drown after grandmother with Alzheimer’s leaves door open

Little boy hugs pizza delivery man goodbye: Shortly after, the boy’s mother makes a tragic discovery

Mom shocked by her baby after birth, her words now spread like forest fire!

Man Mocked For Being With 252 LB Woman

Jelly Roll Stuns Fans with 100-Pound Weight Loss Transformation

Doctors couldn’t believe what they saw during the ultrasound
News Post

Natural Antibiotic: Home Remedy to Relieve Sore Throat

12 Surprising Powers of Calendula officinalis You’ll Wish You Knew Sooner

🥔 Crispy Parmesan Potato Wedges

🧄🧀 Creamy Garlic Parmesan Meatballs

The One Sleep Hack That Could Change Everything: Why Your Bedside Matters

Royal Chocolate Vanilla Sundae

Strawberry Meadow Cake

Rose Garden Strawberry Sundae

Luxury Chocolate & Gold Sprinkle Ice Cream Sundae 🍨✨

Royal Garden Macaron Cake

Midnight Berry Chocolate Loaf Cake

Neighbor calls the cops on two little girls selling lemonade — but she picked the wrong officer

Abandoned puppy gets new owner – check out when he realizes who it is
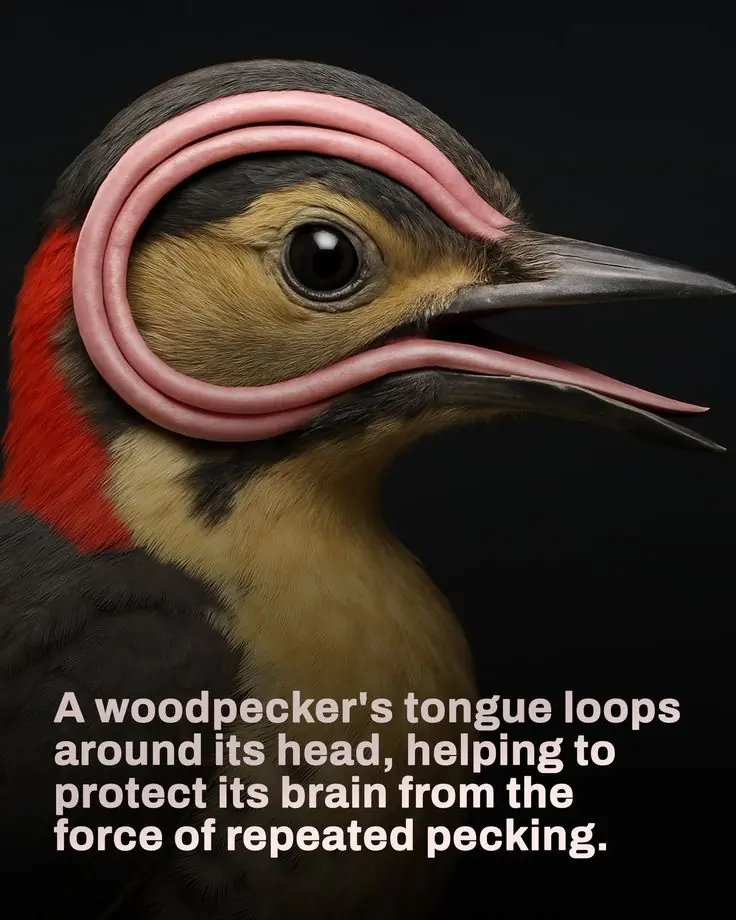
Nature’s Engineering Marvel: The Woodpecker’s Incredible Built-In Safety Mechanism
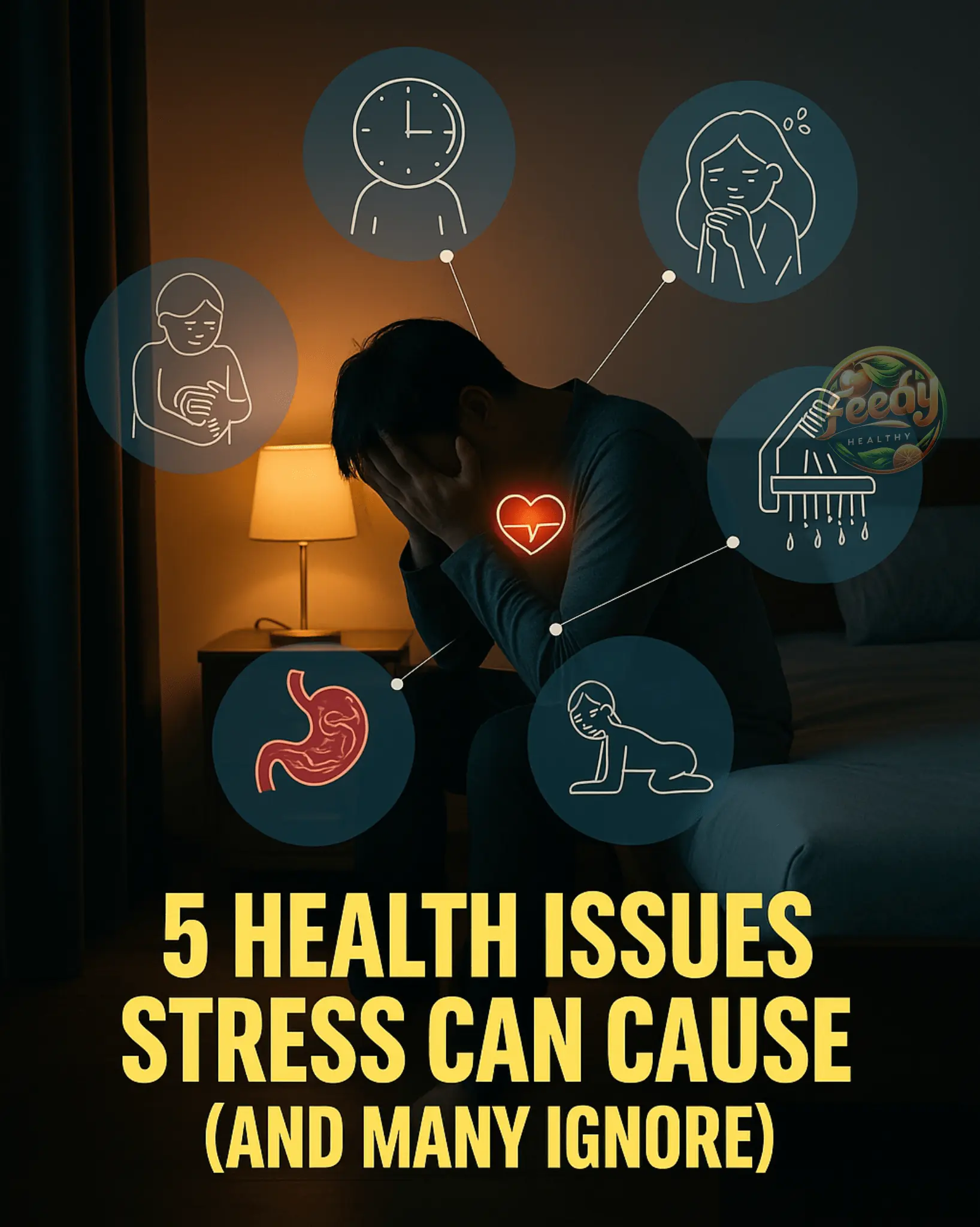
5 Health Issues Stress Can Cause (And Many Ignore)
Unveil the Power of Guava Leaf Tea: Your Secret to Vibrant Health

Okra: The Nutrient-Packed Superfood You Need in Your Diet
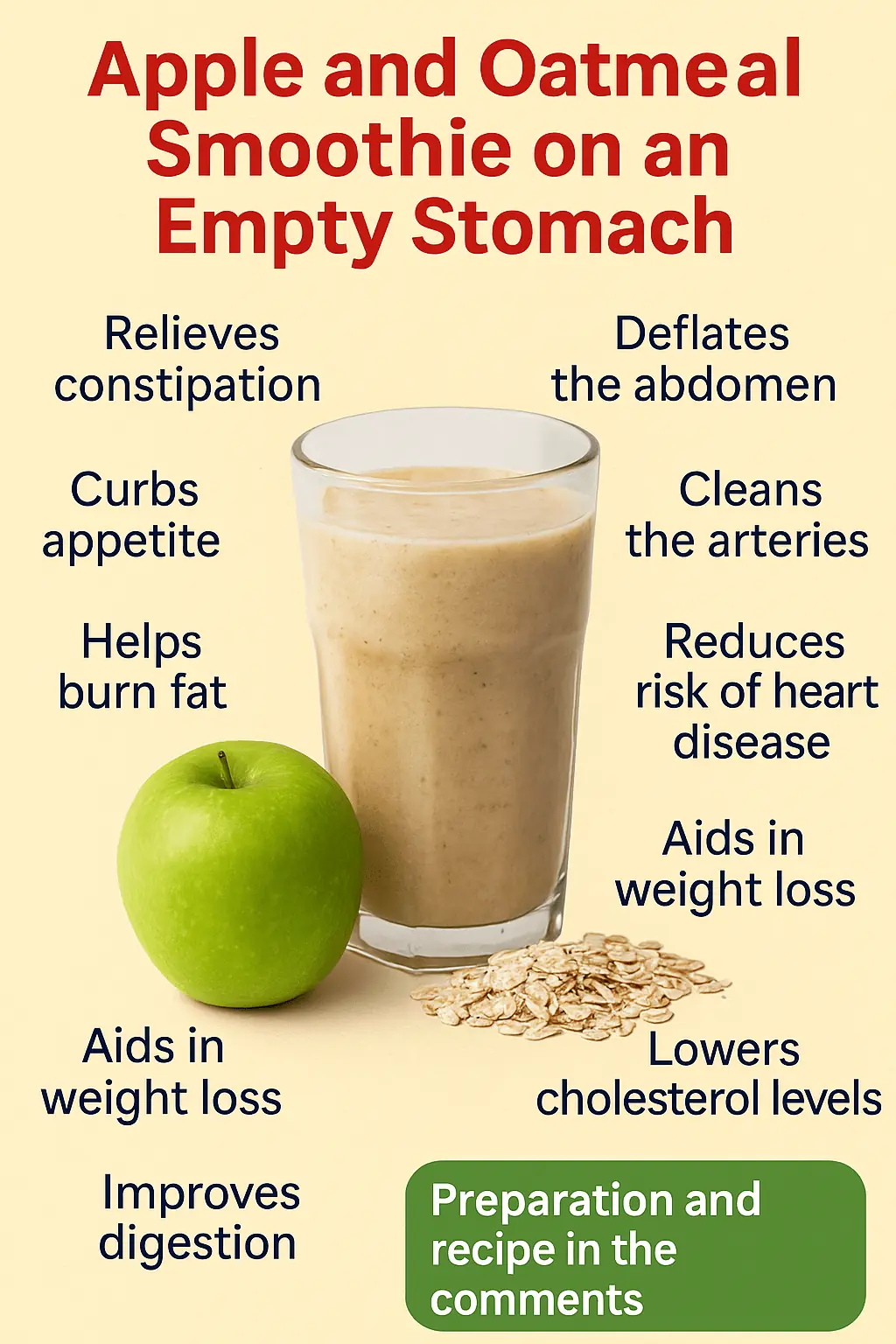
Apple and Oat Smoothie: A Health-Boosting Drink

The Ultimate Wellness Elixir: Why Every Woman Needs This Aidan Fruit Combo