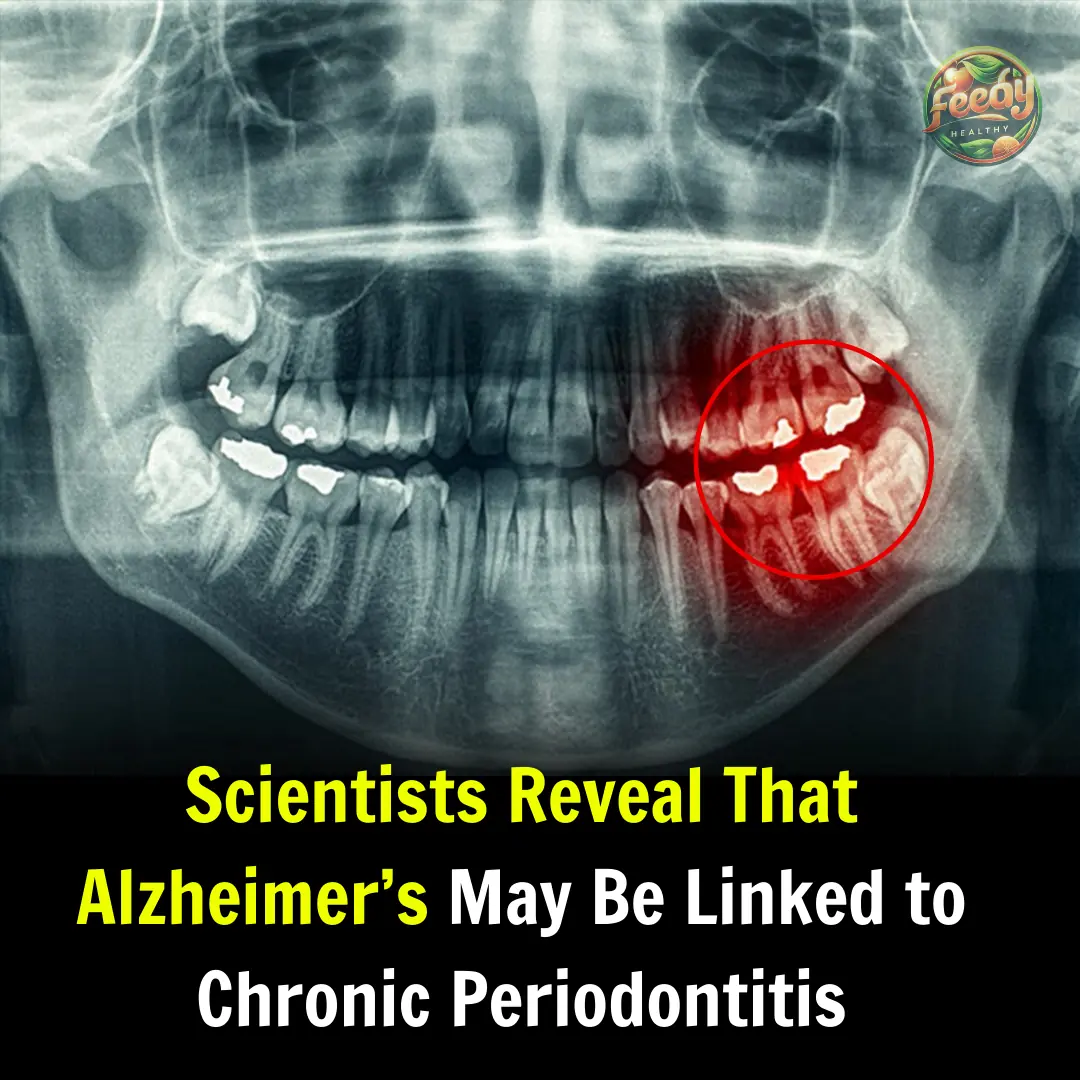
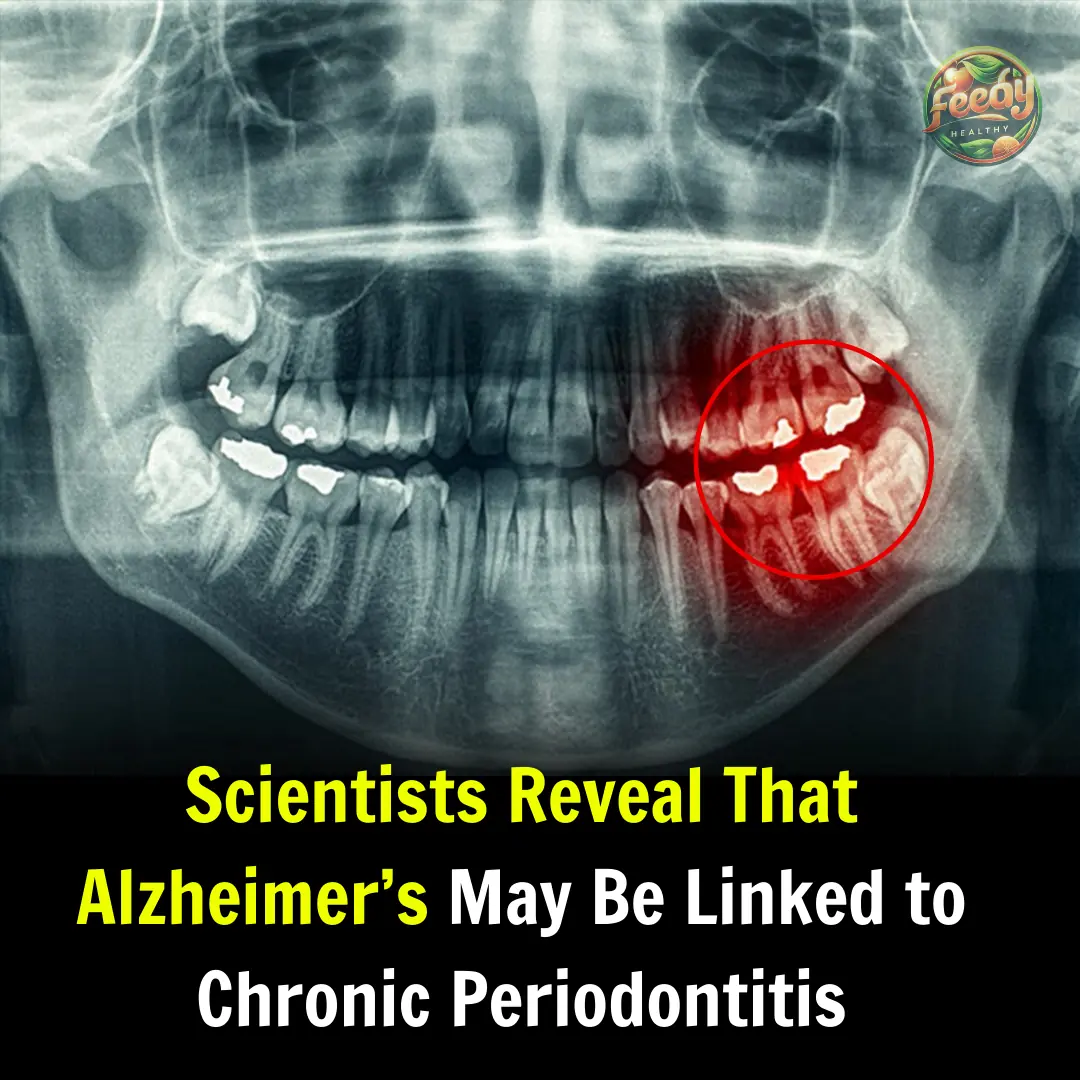
Scientists Reveal That Alzheimer’s May Be Linked to Chronic Periodontitis
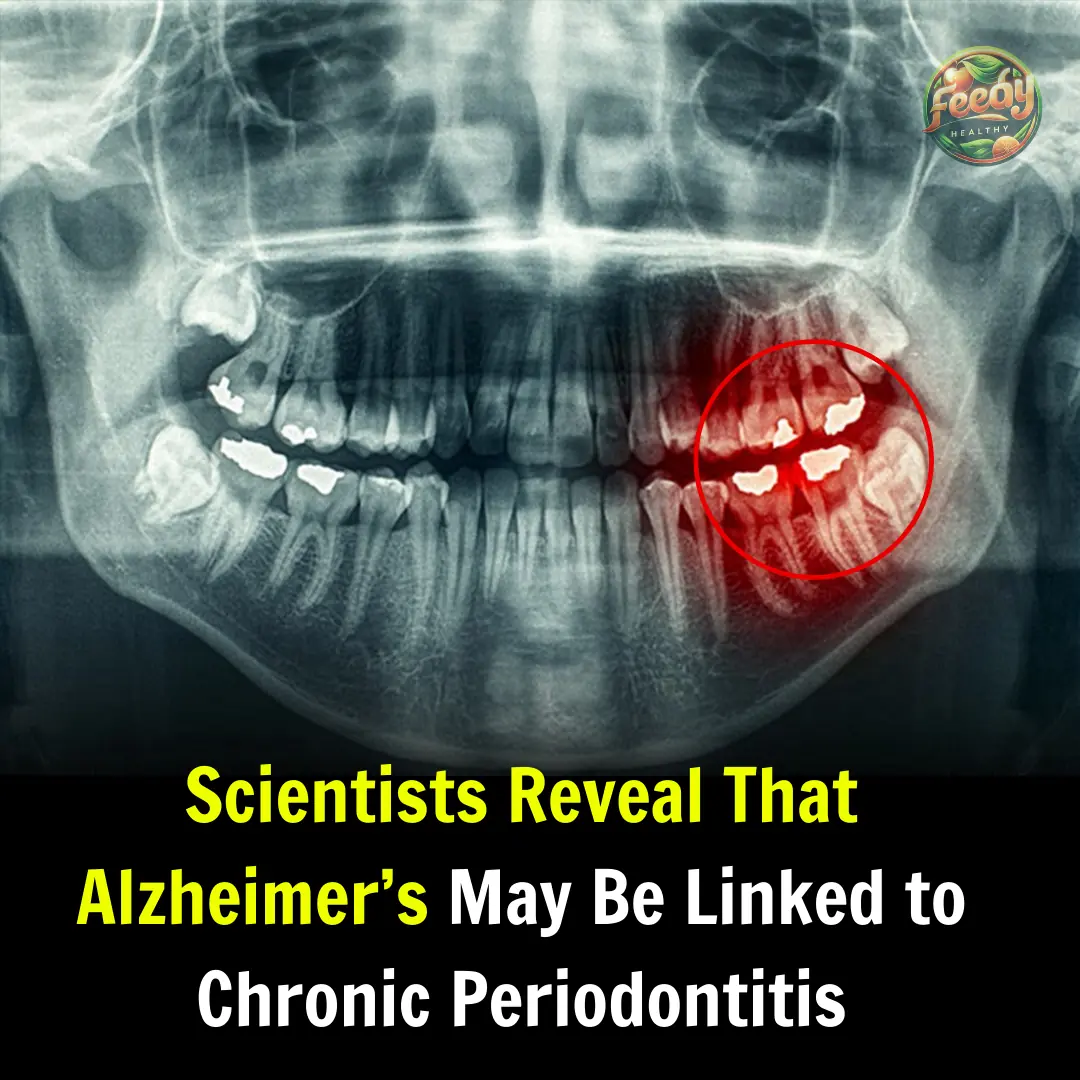
Alzheimer’s, one of the most prevalent neurodegenerative diseases worldwide, affects over 55 million people and is a leading cause of disability among older adults. Characterized by the accumulation of beta-amyloid plaques and neurofibrillary tangles, the disease remains a major challenge for modern medicine due to its multifactorial origins and the limited availability of curative treatments.
📌 Read More: What Are Mouth Ulcers? Causes and Treatments
While genetic and environmental factors have been extensively studied, recent research is now exploring less conventional connections, such as the link between chronic periodontitis and Alzheimer’s. This hypothesis suggests that systemic inflammation triggered by chronic oral infections could play a crucial role in the development of neurodegeneration.
What Is Chronic Periodontitis and How Does It Affect the Body?
Chronic periodontitis is a persistent inflammatory disease affecting the supporting structures of the teeth, including the gums, periodontal ligament, and alveolar bone. It is primarily caused by the accumulation of bacteria in dental plaque, with microorganisms such as Porphyromonas gingivalis playing a key role.
This chronic inflammation not only damages the oral cavity but also has systemic effects, triggering immune responses that impact distant organs. Recent studies suggest that activated immune cells and pro-inflammatory cytokines like tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6) may contribute to conditions such as cardiovascular diseases, diabetes, and potentially Alzheimer’s. Additionally, periodontal disease can exacerbate microbiome imbalances, creating a vicious cycle of inflammation and deterioration in other systems.
Furthermore, research has shown that periodontal bacteria can trigger persistent inflammatory responses that weaken the immune system, allowing pathogens to enter the bloodstream. This poses risks to vital organs, including the brain, increasing the possibility of a direct link to Alzheimer’s.
The Link Between Alzheimer’s and Chronic Periodontitis
Recent studies have identified a connection between oral health and brain health, proposing that chronic inflammation caused by periodontal diseases may be a risk factor for Alzheimer’s.
One major culprit is the bacterium Porphyromonas gingivalis, which produces toxins called gingipains. These toxins can penetrate the blood-brain barrier, triggering neuroinflammation and contributing to the accumulation of beta-amyloid plaques, a hallmark of Alzheimer’s disease.
A study published in the Journal of Preventive Alzheimer’s Disease found that individuals with periodontitis are more likely to develop cognitive decline. Additionally, inflammatory markers associated with periodontal disease, such as IL-1β, have also been detected in the brains of Alzheimer’s patients, reinforcing the hypothesis of a causal association.
These findings suggest that cognitive deterioration could be accelerated by systemic inflammation originating in the mouth. Therefore, oral health should not be overlooked in the fight against neurodegenerative diseases.
Porphyromonas Gingivalis: The Bacteria Involved in Neuroinflammation
Porphyromonas gingivalis is a gram-negative anaerobic bacterium that plays a crucial role in the pathology of chronic periodontitis. Studies have shown that this bacterium can not only colonize the oral cavity but also invade other tissues, including the brain.
Once in the brain, it releases toxins that activate microglial cells and astrocytes, triggering neurotoxic inflammation.
According to a study published in Critical Reviews in Microbiology, outer membrane vesicles from P. gingivalis facilitate the entry of its toxins into the central nervous system. These toxins stimulate the formation of beta-amyloid plaques and neurofibrillary tangles, which are hallmarks of Alzheimer’s disease, promoting neuronal death and progressive cognitive decline.
Moreover, this bacterium has been found to activate immune pathways that exacerbate inflammatory responses, amplifying neuronal damage. This underscores the importance of early interventions to control infection and mitigate systemic effects.
How Chronic Inflammation Contributes to Alzheimer’s Development
Chronic inflammation is a key factor in the progression of Alzheimer’s disease. The persistent presence of pro-inflammatory cytokines creates a neurotoxic environment, impairing neuronal function and facilitating amyloid plaque buildup in the brain.
Additionally, studies have shown that bacterial toxins can disrupt the blood-brain barrier, allowing pathogens and inflammatory molecules to enter the brain.
A study conducted on animal models revealed that infection with P. gingivalis increases levels of interferons and innate immune system proteins like IFITM3, which accelerate beta-amyloid plaque formation and worsen cognitive impairment. This suggests that controlling chronic inflammation could be a viable strategy for preventing or delaying Alzheimer’s symptoms.
Furthermore, research has demonstrated that interactions between oral bacteria and neural cells can modulate gene expression in the brain, affecting key processes such as neurogenesis and synaptic plasticity. This highlights how an apparently localized infection can have profound neurological consequences.
Prevention and Treatment: Maintaining Oral Health to Protect the Brain
These findings emphasize the importance of oral health as a preventive strategy against Alzheimer’s disease. The following measures may help reduce the risk:
✔ Proper oral hygiene: Regular brushing, flossing, and routine dental check-ups are essential to prevent chronic periodontitis.
✔ Early treatment: Identifying and treating periodontal infections early can reduce systemic inflammation and its long-term effects.
✔ Research into new therapies: The development of gingipain inhibitors and targeted treatments could offer innovative options to mitigate the impact of periodontal bacteria on brain health.
Additionally, raising awareness about the link between oral health and neurodegenerative diseases could lead to significant lifestyle changes. It is crucial for both healthcare professionals and the general public to understand that a healthy mouth may be the key to a healthy brain.
News in the same category

Blood Sugar Fluctuations Over 24 Hours – How Does It Work at Different Times of the Day?

Blood Sugar Fluctuations Over 24 Hours – How Does It Work at Different Times of the Day?

What Are the Effects of Sleeping After 11 PM for a Long Time? The Consequences May Only Be Felt by Yourself!
Doctors Successfully Cure a Fatal Genetic Disease in a Fetus for the First Time

Useful aspirin tricks that every woman should know

7 Red Flags That Show Your Body Lacks Essential Nutrients

Foods That Are Unsuitable for People with High Blood Pressure – Avoid These Now!

Can Eating Walnuts Clean Your Blood Vessels? Reminder: Protect Your Blood Vessels – Don’t Overlook These Foods!

Heard That Milk Is Full of Preservatives, Toxic, and Causes Cancer? What’s the Truth? Let’s Find Out!

Ranking of Weight-Gaining Foods: Rice and Steamed Buns Are Not on the List – Avoid These Foods If You Want to Lose Weight!

Is Drinking Alcohol in Moderation Safe? Doctor Warns: These 4 Groups of People Should Avoid Alcohol Completely!

Frequent Recurrence of Canker Sores: Beyond "Internal Heat," 6 Possible Causes to Know and Prevent

How to Prevent and Treat Stroke Caused by Atrial Fibrillation? Protecting Our Health

25 Years Old, Passing Gas Dozens of Times a Day – What’s Going On? Doctor Warns: 3 Unusual Signs Not to Ignore
9 Health Signs Your Feet Might Reveal About Your Body
Peru Makes History: The First Baby Born Using External Egg Maturation Technology

Fatty Liver: Causes, Symptoms, Treatment & Home Remedies
Discovery of a Highly Contagious and Virulent HIV Variant
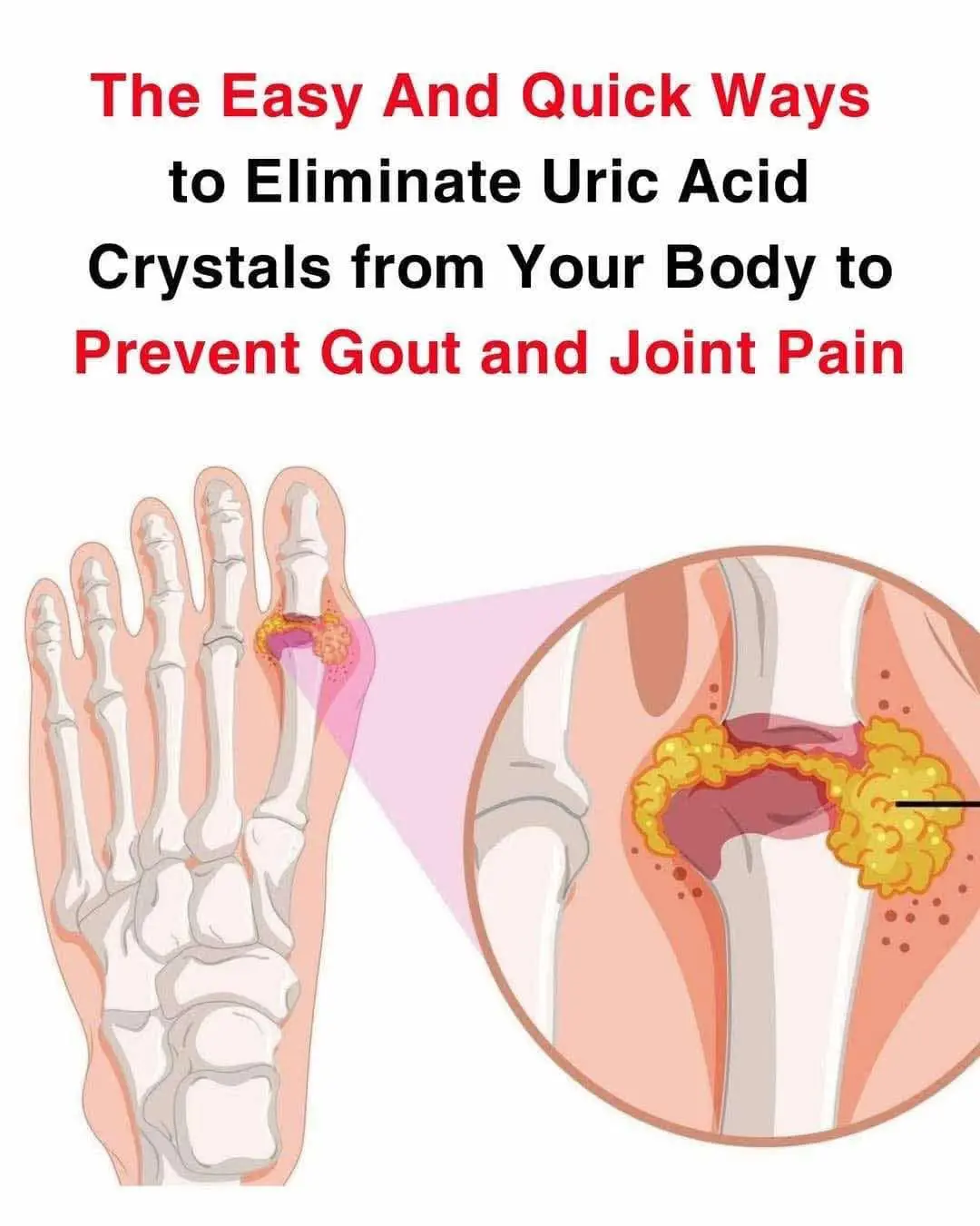
How to help naturally relieve gout and joint pain
News Post

9 Foods You Can Grow In Buckets All Year

The whole world is celebrating the discovery of a vegetable

Dad of 4 Living in Tent Gives Last $2 to Stranger at Gas Station, Wakes up Owning a Big Company — Story of the Day
Paternal Stress Leaves Marks on Sperm

An Unforgettable 80th Birthday: A Father, A Daughter, and a Dark Secret.

12 Signs of Low Blood Sugar: Symptoms You Should Never Ignore Uncategorized

Natural Recipe with Watermelon, Carrot, Beetroot, and Ginger

My Best Friend Married My Ex-Husband — Then She Called Me in the Middle of the Night, Terrified.
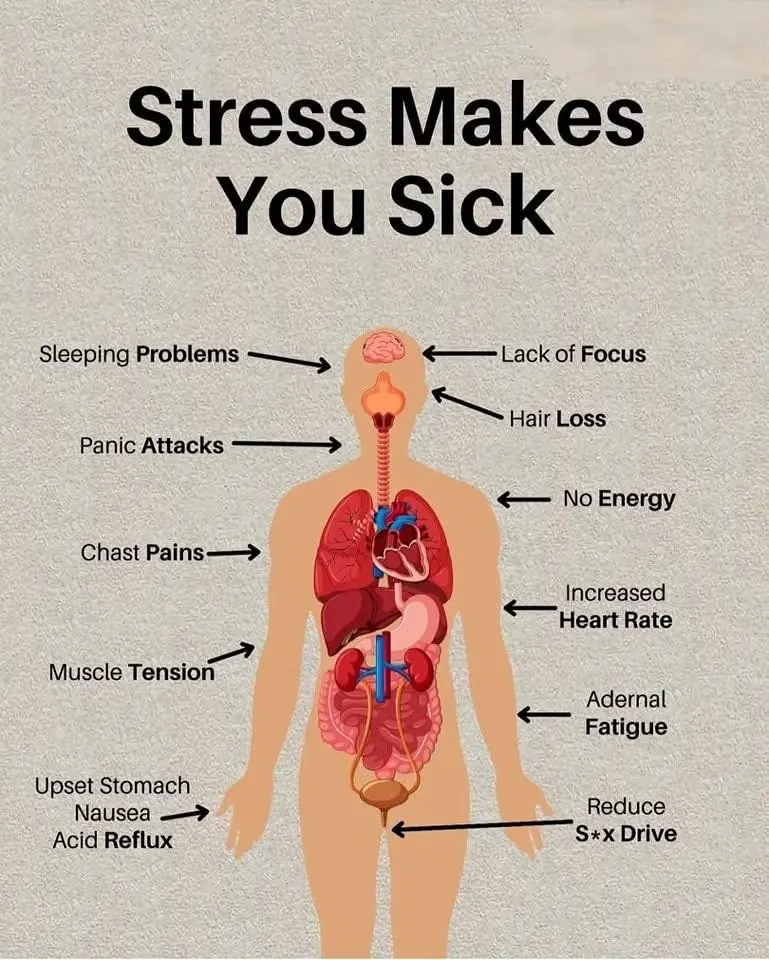
How Stress Affects Your Health & Ways to Manage It

Medicinal Uses of Jatropha Curcas: Recipes, Properties, and Precautions

I Gave Money to a Poor Woman with a Baby — And the Next Morning, I Was Shocked to Find Her at My Husband’s Grave.

Unlock the Power of Garlic: Chew Two Cloves Daily to Say Goodbye to Health Problems

Feel Like a Teenager Again: The Incredible Joint-Healing Power of Bay Leaves
Doctor warn of these 8 food that cause cancer

I Almost Left after Seeing Our Baby – But Then My Wife Revealed a Secret That Changed Everything

30 Incredible Benefits of Dandelion: Nature’s Hidden Gem

AS A SINGLE MOM WORKING AT A DINER, I LOST SIGHT OF MY SON—WHAT HE SAID TO A FIREFIGHTER LEFT US ALL IN TEARS

Blood Sugar Fluctuations Over 24 Hours – How Does It Work at Different Times of the Day?
