
Doctors Successfully Cure a Fatal Genetic Disease in a Fetus for the First Time

Spinal muscular atrophy (SMA) has historically been one of the most devastating genetic diseases, severely affecting the motor abilities of those who suffer from it. Until recently, postnatal treatments had improved the life expectancy of patients, but there was no effective strategy to prevent the disease's progression before birth.
However, a recent study published in The New England Journal of Medicine documents a groundbreaking case: the prenatal administration of the drug Risdiplam has, for the first time, prevented the onset of a lethal form of SMA in a fetus. This achievement sets a historic precedent in fetal medicine and intrauterine gene therapy.
What is Spinal Muscular Atrophy (SMA)?
Spinal muscular atrophy, commonly known as SMA, is a group of neuromuscular disorders of genetic origin that directly affect the motor neurons of the spinal cord. The gene involved in most cases is SMN1, responsible for producing a crucial protein for motor neuron survival, known as the SMN protein.
When this gene undergoes mutations or deletions, the body fails to produce enough SMN protein, leading to progressive muscle weakness and, in severe cases, early death. The severity of SMA is classified into four types (1, 2, 3, and 4), with type 1 being the most severe. It manifests within the first few months of life, causing significant muscle weakness and respiratory difficulties, which can be fatal without early intervention.
Despite the complexity of this disease, the human body has a secondary gene, SMN2, which also produces the SMN protein, albeit in lower amounts due to RNA splicing alterations. The latest SMA treatments focus on enhancing SMN2 function to increase SMN protein levels, thereby maintaining motor neuron activity and slowing disease progression.
The Role of Risdiplam in SMA
Risdiplam is an oral drug approved by health authorities in various countries for the treatment of SMA. Its primary function is to modulate the splicing of the SMN2 gene, enabling it to produce higher-quality SMN protein to compensate for the lack of SMN1.
Read More: How Do Fetuses Breathe in the Womb?
The effectiveness of Risdiplam has been documented in multiple clinical trials, especially in patients with SMA type 1 who receive treatment after birth. However, the recently reported case suggests that the drug can also be administered in the third trimester of pregnancy, crossing the placental barrier to reach the fetus and begin protecting motor neurons before they suffer irreversible damage.
The First Case of Intrauterine Therapy
The study authors presented the case of a mother whose fetus was prenatally diagnosed with SMA type 1. The diagnosis was made through amniocentesis, which revealed the absence of the SMN1 gene and the presence of two copies of SMN2, a genetic profile associated with the most severe form of the disease.
- Genetic profile: Confirmation of SMA type 1 due to SMN1 deficiency.
- Intervention timing: 32nd week of pregnancy.
- Drug administered: Risdiplam.
- Mode of administration: Oral intake by the mother, allowing the drug to reach the fetal environment.
During this period, doctors closely monitored the pregnancy and the health of both the mother and the fetus. Regular ultrasounds were performed to ensure proper fetal development and activity, alongside blood and amniotic fluid tests to measure Risdiplam levels and its effects on SMN protein production.
Post-Birth Progress
The baby was born around the 39th week of pregnancy and continued receiving oral Risdiplam after birth. At the last recorded evaluation (approximately 30 months of age), there were no signs of SMA: no hypotonia, muscle weakness, or respiratory problems characteristic of type 1 SMA.
Some medical findings, such as a minor heart septum defect and slight visual issues, were attributed to events that occurred early in embryonic development, prior to drug administration. These anomalies do not appear to be related to SMA or side effects of Risdiplam.
The Importance of Early Detection
The key takeaway from this report is the critical importance of prenatal detection. While therapies already existed to improve postnatal outcomes for SMA patients, this intrauterine intervention demonstrates that an even earlier start of treatment could prevent motor neuron loss and avert severe symptoms.
- Genetic testing: Amniocentesis was essential for fetal diagnosis, allowing the identification of the genetic mutation responsible for SMA type 1.
- Advantage of early diagnosis: By confirming the condition in time, doctors were able to schedule Risdiplam administration before motor neurons began degenerating.
- Constant monitoring: A strict schedule of ultrasounds and laboratory tests ensured the safety of both mother and fetus, assessing treatment efficacy and potential risks.
Applications in Fetal Medicine
The possibility of treating fatal genetic diseases before birth opens new frontiers in fetal medicine. Until now, intrauterine interventions have mainly focused on fetal surgeries for physical malformations (such as spina bifida repair). However, the SMA case highlights the potential of pharmacological therapies acting at the molecular level.
- New therapeutic horizons: The evidence that Risdiplam can cross the placental barrier and positively impact the fetus encourages future research into other genetic diseases.
- Expanded clinical trials: To confirm the consistent safety and efficacy of this procedure, larger studies with long-term follow-ups are required. It is essential to assess the stability of neuromuscular recovery and rule out potential side effects in later developmental stages.
Future Advances in Gene Therapy
The success of this case motivates scientists and medical institutions to further explore gene-editing and cell therapy before birth. Techniques like CRISPR-Cas9, which allow precise DNA mutation corrections, could be combined with drugs like Risdiplam to offer more comprehensive and definitive solutions.
Additionally, continuous monitoring of blood markers and evaluating neurofilament and SMN levels in both the mother and newborn could help refine dosage and timing of interventions. In the future, this personalized approach could be adapted to different SMA variants and other genetic disorders.
Conclusion
The remarkable achievement of "curing" a fatal genetic disease before birth in a single case opens a completely new chapter in perinatal and genetic medicine. Beyond preventing the devastating effects of SMA type 1, this prenatal intervention with Risdiplam demonstrates the real possibility of acting on the fetal genome and physiology before the disease manifests symptoms.
Although further research is necessary to confirm the large-scale safety and efficacy of this treatment, this breakthrough marks a turning point in the approach to SMA and other genetic disorders. With earlier diagnosis and targeted molecular therapy, the hope is that more children will be born free from severe diseases that were once considered unavoidable.
News in the same category


Blood Sugar Fluctuations Over 24 Hours – How Does It Work at Different Times of the Day?

What Are the Effects of Sleeping After 11 PM for a Long Time? The Consequences May Only Be Felt by Yourself!
Doctors Successfully Cure a Fatal Genetic Disease in a Fetus for the First Time

Useful aspirin tricks that every woman should know

7 Red Flags That Show Your Body Lacks Essential Nutrients

Foods That Are Unsuitable for People with High Blood Pressure – Avoid These Now!

Can Eating Walnuts Clean Your Blood Vessels? Reminder: Protect Your Blood Vessels – Don’t Overlook These Foods!

Heard That Milk Is Full of Preservatives, Toxic, and Causes Cancer? What’s the Truth? Let’s Find Out!

Ranking of Weight-Gaining Foods: Rice and Steamed Buns Are Not on the List – Avoid These Foods If You Want to Lose Weight!

Is Drinking Alcohol in Moderation Safe? Doctor Warns: These 4 Groups of People Should Avoid Alcohol Completely!

Frequent Recurrence of Canker Sores: Beyond "Internal Heat," 6 Possible Causes to Know and Prevent

How to Prevent and Treat Stroke Caused by Atrial Fibrillation? Protecting Our Health

25 Years Old, Passing Gas Dozens of Times a Day – What’s Going On? Doctor Warns: 3 Unusual Signs Not to Ignore
9 Health Signs Your Feet Might Reveal About Your Body
Peru Makes History: The First Baby Born Using External Egg Maturation Technology

Fatty Liver: Causes, Symptoms, Treatment & Home Remedies
Discovery of a Highly Contagious and Virulent HIV Variant
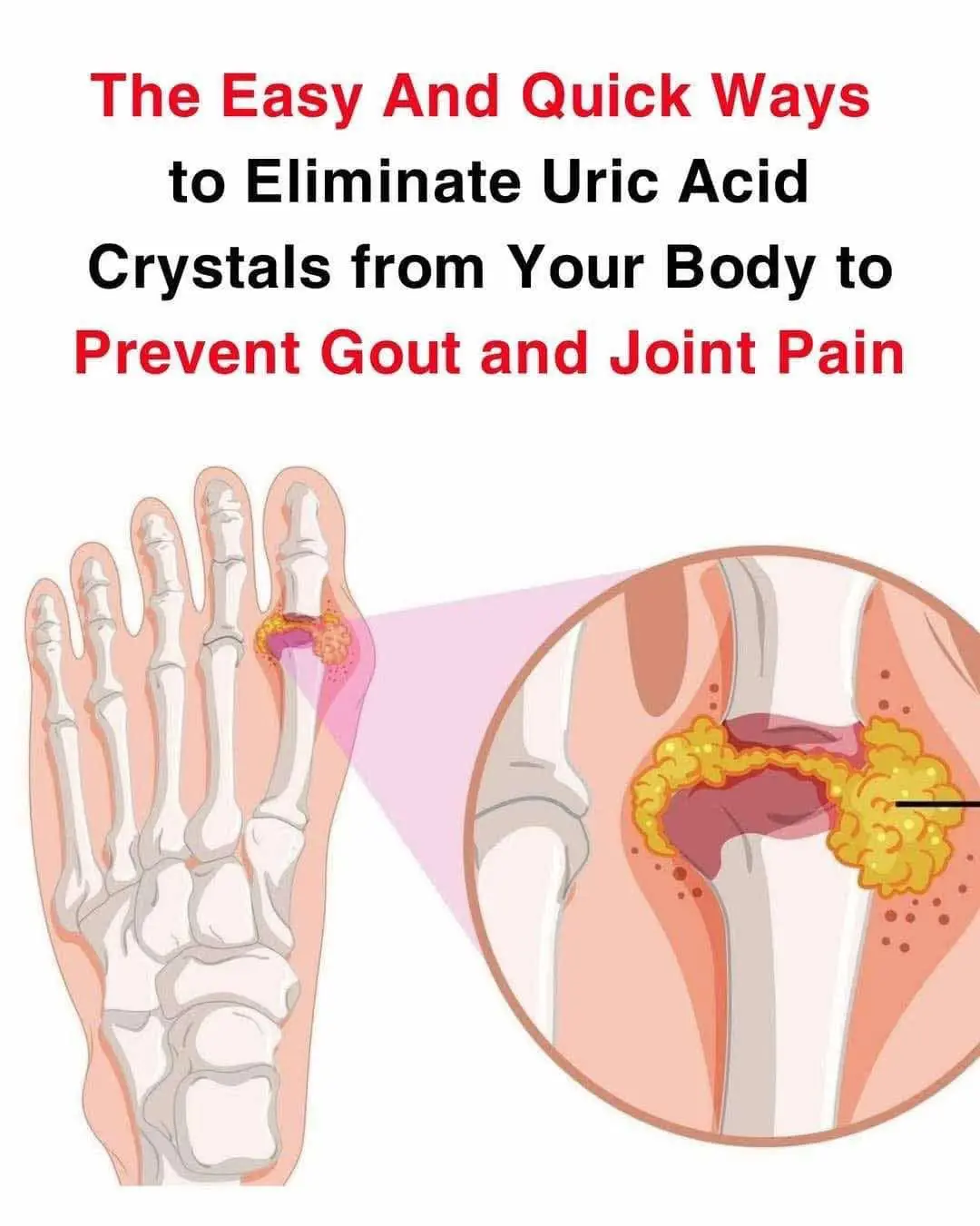
How to help naturally relieve gout and joint pain
A rogue ranger is documenting every National Park Service firing
News Post

Medicinal Uses of Jatropha Curcas: Recipes, Properties, and Precautions

I Gave Money to a Poor Woman with a Baby — And the Next Morning, I Was Shocked to Find Her at My Husband’s Grave.

Unlock the Power of Garlic: Chew Two Cloves Daily to Say Goodbye to Health Problems

Feel Like a Teenager Again: The Incredible Joint-Healing Power of Bay Leaves
Doctor warn of these 8 food that cause cancer

I Almost Left after Seeing Our Baby – But Then My Wife Revealed a Secret That Changed Everything

30 Incredible Benefits of Dandelion: Nature’s Hidden Gem

AS A SINGLE MOM WORKING AT A DINER, I LOST SIGHT OF MY SON—WHAT HE SAID TO A FIREFIGHTER LEFT US ALL IN TEARS

Blood Sugar Fluctuations Over 24 Hours – How Does It Work at Different Times of the Day?

Blood Sugar Fluctuations Over 24 Hours – How Does It Work at Different Times of the Day?

What Are the Effects of Sleeping After 11 PM for a Long Time? The Consequences May Only Be Felt by Yourself!

10 Foods That Are Making Your Belly Bigger

Do You Know the 10 Superfoods That Kill Cancer Cells?

My Mother’s Intuition Uncovered a Secret No One Expected—And I Refused to Stay Silent

Useful aspirin tricks that every woman should know

Title: Daughter’s Discovery in Dad’s Suitcase Shatters Family

Is Milk Full of Preservatives, Toxic, and Cancer-Causing? Is It True? Let’s Find Out!

An old man always bought two movie tickets, then I learned the heartwarming reason why.
